After a long day on your feet, you have just finally fallen asleep. Suddenly, you wake up with terrible leg and foot cramping, again! That’s it, you’ve had enough. As if the leg swelling, aching, and pain aren’t enough during the day, the lack of sleep at night is the last straw. It’s decided – time to visit your local vein specialist to see what can be done to provide some relief.
What to Expect at Your Very First Vein Consultation
After completing your new patient paperwork and providing insurance information to the front desk staff, you are brought back into a room, asked to change into not so fashionable but comfortable blue shorts. Your vein physician, specializing in the diagnosis and treatment of vein disease, meets with you and discusses your medical history. They will then discuss any family history of vein disease, past surgeries, prior known vein or vascular disease, current symptoms, and perform a thorough physical examination of your legs. Since you have symptoms of vein disease, they will order a thorough ultrasound of your legs, which is then scheduled at your request on another date that works best for you.
What to Expect at Your First Vein Ultrasound Appointment
Ultrasound has changed the medical landscape in the last 35 years. With rapid technological advancement, ultrasound machines are now smaller, more accurate, more sensitive, and portable. Ultrasound, in the hands of a trained, credentialed sonographer, is a diagnostic tool that is the Gold Standard for the diagnosis of vein disease. This technology allows for the use of sound waves (no radiation) to help image tissues in your legs. The exam lasts 60-75 minutes, is painless, and provides information that is instrumental for your vein treatment plan.
During this appointment, the sonographer will introduce themselves and will let you know what you can expect from this appointment. First, they will look at some of the deep veins in your legs to ensure you do not have a deep vein thrombosis, then they will focus on assessing the superficial venous system, the system in which vein disease is commonly the source of your symptoms. All major veins in this venous system will be assessed from your groin to your ankle on the inside and front of your leg, on the outside of your leg, and then on the back of your leg. You will feel the warm (and then cooling) ultrasound gel on your leg. They will press the ultrasound probe into your leg, and then you will feel them squeezing your leg, usually at the calf, and sometimes on the thigh.
As they scan, you may notice that they will also create a “map” or diagram of your veins, drawing abnormal veins in red and leaving normal veins in black and white. This vein map, along with the ultrasound images, represents the severity and extent of your vein disease, which veins are affected, and therefore which treatment options are best for you.
What the Results of Your Vein Ultrasound Mean
Medium Vein Disease (MVD)
If your symptoms are from medium vein disease (MVD), meaning you suffer from spider veins and telangiectasias (the small blue/green veins that are just beneath the skin), your treatment option will most likely be sclerotherapy. Sclerotherapy must be performed by extensively trained registered nurses, nurse practitioners, physician assistants, or physicians. In this procedure, a sclerosant solution is injected directly into the vein using tiny needles connected to a syringe via sight. During this procedure, you will feel some burning and stinging as the medication begins activating in the vein. The veins then spasm, shut down and divert blood flow to other, healthy veins. Typically, 2-4 treatment sessions are recommended.
Large Vein Disease (LVD)
If your symptoms are from large vein disease, you will require a few additional procedures. The best treatment plan is “source to course”. This means that first, the source is treated, then the remainder of the disease is treated. When you think of the superficial venous system, imagine a tree. The trunk of the tree are the saphenous veins, also known as truncal veins. If these veins are diseased, they are often the “source” of disease, meaning they are treated first. Once they are treated, your vein doctor will move on to the branches of the tree which are the varicose veins, or tributaries. Finally, the leaves, which are the spider veins and reticular veins will be treated.
If you were to start with the spider vein instead of the saphenous veins, the spider veins would still be under a lot of pressure from the larger saphenous vein and either reopen, or the saphenous veins would create new spider veins. Another way to think of vein disease is like a backwards river; the river (the saphenous veins) pushes and creates the tributaries, which then push and create the spider veins. So, the treatment of vein disease is a process, but one that when done properly, can have great results.
Chronic Venous Insufficiency Treatment Options
Let’s explore the different options for vein treatment, using the tree analogy.
Recommended treatments for truncal veins
First, let’s focus on treating the trunk of the tree, or the truncal veins. The recommended vein treatment options for these veins are as follows:
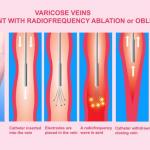
Notice that all three of the options share two words: endovenous and ablation. Endovenous means within a vein, and ablation means the damage or destruction of a structure, in this case, a vein. The veins are not surgically treated or removed, but rather, shut down so that blood is diverted to other, healthy veins. The different treatment options refer to the means used to damage the vein, causing it to shut down. Both LASER and radiofrequency vein treatment use heat, and adhesive uses, you guessed it – glue! These procedures are performed using ultrasound guidance and must be performed by extensively trained physicians like our team of experts at USA Vein Clinics.
Recommended treatments for varicose and tributary veins
Once these veins are shut down, the next step is to take care of the branches of the tree: the varicose and tributary veins. The recommended vein treatment options for these veins are as follows:
- Ultrasound-Guided Sclerotherapy
- Ambulatory Phlebectomy
Ultrasound-guided sclerotherapy is exactly as described: sclerotherapy that is performed with the use of ultrasound. Often, a foamed sclerosant is used to increase effectiveness. You may feel a slight stinging during the injection from the needlestick and possibly some itching or burning following the injection as the medication activates within the vein. This procedure must be performed by extensively trained nurse practitioners, physician assistants, or physicians.
Next is ambulatory phlebectomy, also known as microphlebectomy, or simply phlebectomy. This is the surgical removal of large, tortuous varicose veins easily seen at the surface of the skin. A series of small incisions are made, a small hook is inserted below the skin and used to pull the vein out, and then it is surgically removed. In the hands of trained and skilled professionals, this is an excellent procedure option for treating chronic venous insufficiency. This procedure must be performed by extensively trained physicians.
All of these vein procedures are minimally invasive, performed in the physician’s office, and you are encouraged to walk and return to most normal activities following each procedure – with no downtime!
What to Expect Following Chronic Venous Insufficiency Treatment
It is important to keep in mind that chronic venous insufficiency, or varicose vein disease, is progressive and that there is no cure. Without treatment, it will continue to get worse, but even with treatment, you may need additional treatments. One physician explains it as such: “Think of it like a car, we see what’s going on and then rebuild the engine. After that, you should bring the car back in once a year to see if it needs an oil change.”
Adherence to the prescribed treatment option based on accurate and thorough ultrasound will treat the vein disease you have today but over time, it is not uncommon for new veins to appear. The aim is to prevent your signs and symptoms from being as bad as they were when you first came to the office. Treating the source of your vein disease should significantly slow down the process of developing new varicose veins, but each person is unique, as is their disease process.
Importance of Annual Vein Checkups for Continued Improvement
Regular check-ins and being aware of symptoms are key. Remember, “if you feel something, say something”. If you begin to see or feel any of the signs and symptoms that brought you to the office in the first place, call your team of vein specialists and set up an appointment.
Vein Disease is Progressive – Take the Right Steps to Treat Symptoms
Know that you are not alone! Vein disease is common and now well understood. CVI, or chronic vein disease, is easily diagnosed, treatment options are quick, effective, usually have minimal pain, if any, with little to no downtime, and are covered by most insurance. Remember that spider veins or unexplained symptoms can be an indication of varicose vein disease, and treating spider veins, prior to ruling out a source, can lead to treatment failures. Although vein disease is progressive and there is no cure, treatments can greatly impact your quality of life.
So, what are you waiting for? Listen to your legs. Contact us if you are experiencing any of the following symptoms:
-
- Achy legs
- Leg heaviness
- Restless legs
- Throbbing
- Cramping
- Skin discoloration in your legs or ankles
- Leg ulcers
- Bulging veins or even spider veins
Find a vein specialist near you and set up a consultation. You may only be an ultrasound away from knowing how you can get your legs back!