When most people think about vein problems, they picture bulging varicose veins or clusters of tiny spider veins on the legs. But did you know that vein disease can also affect the smaller, deeper veins you can’t see? This condition—known as small vein disease—can cause many of the same uncomfortable symptoms and long-term risks as visible vein disease, even though it’s hidden beneath the surface.
Understanding Vein Function
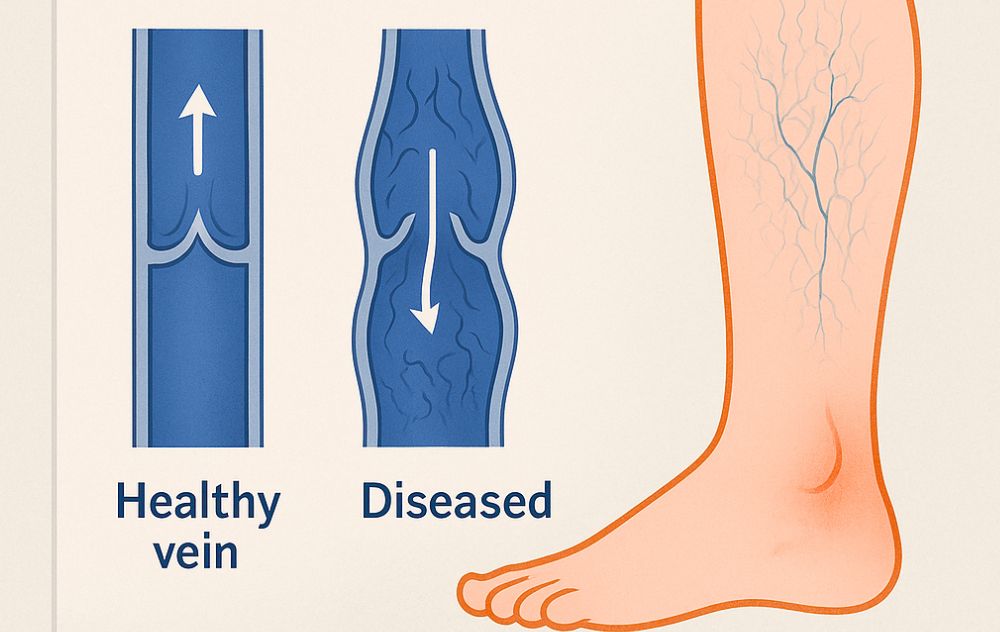
Your veins play a vital role in carrying blood from your body back to your heart. To keep blood flowing in the right direction, veins rely on tiny one-way valves. When these valves weaken or become damaged, blood can pool in the legs, increasing pressure within the veins. This condition is called chronic venous insufficiency (CVI)—and it’s the root cause of many vein problems, including small vein disease.
What Exactly Is Small Vein Disease?
Small vein disease refers to circulation problems in the tiny veins just under the skin or within the deeper layers of tissue. These smaller veins may not be visible from the outside, but they can still leak blood backward (reflux), leading to inflammation, pain, swelling, and discoloration.
Unlike larger varicose veins, small vein disease often goes unnoticed because there are few outward signs. However, it can significantly impact your leg health and comfort over time.
Common Symptoms of Small Vein Disease
Even if you don’t see visible veins, you might still experience symptoms such as:
-
Heaviness or fatigue in the legs after standing or sitting for long periods
-
Swelling around the ankles or calves
-
Aching, burning, or cramping sensations
-
Itchy or dry skin near the lower legs or feet
-
Skin discoloration or thickening, especially near the ankles
-
Restless legs or nighttime discomfort
Because these symptoms mimic other conditions, small vein disease often goes undiagnosed until more serious complications arise—such as ulcers or deep vein thrombosis (DVT).
Who Is at Risk?
Several factors can increase your risk of developing small vein disease, including:
-
Family history of varicose veins or vein disease
-
Standing or sitting for long hours at work
-
Obesity or being overweight
-
Pregnancy and hormonal changes
-
Aging
-
Prior leg injury or surgery
-
Smoking
Even if you lead a healthy lifestyle, genetics alone can make you more prone to developing venous insufficiency.
Small Vein Disease vs. Small Vessel Disease: What’s the Difference?
Although the names sound similar, small vein disease and small vessel disease affect entirely different parts of the body. Understanding the distinction can help patients recognize symptoms and get the right type of care.
Small Vein Disease refers to problems in the superficial or deeper veins of the legs, often involving poor blood flow due to weakened vein valves. This can lead to visible spider veins, reticular veins, or varicose veins, along with symptoms like leg pain, swelling, heaviness, and fatigue. Over time, untreated vein disease can cause skin discoloration or even ulcers. Treatment typically involves minimally invasive vein procedures that restore healthy circulation and relieve discomfort.
Small Vessel Disease (SVD), on the other hand, affects the tiny arteries (arterioles) of the heart or brain, not the veins. In the heart, it’s called coronary microvascular disease, and it restricts blood flow to the heart muscle, causing chest pain and fatigue similar to coronary artery disease. In the brain, small vessel disease can lead to strokes or cognitive decline over time. This condition is managed through cardiac or neurological care, focusing on improving blood flow and controlling risk factors like high blood pressure, cholesterol, and diabetes.
In short, small vein disease impacts the veins—especially in the legs—while small vessel disease affects the arteries supplying vital organs. Both involve circulation issues but require very different specialists and treatments.
Are Spider Veins and Small Vein Disease the Same?
Not exactly — but they’re closely related. Spider veins are often a visible sign of small vein disease, which affects the tiny veins just below the skin’s surface.
Spider veins appear as thin, web-like clusters of red, blue, or purple lines, commonly found on the legs or face. While many people view them as a cosmetic concern, they can also indicate underlying venous insufficiency — a condition where small veins struggle to return blood to the heart efficiently. When the valves in these veins weaken, blood pools and pressure builds, leading to visible spider veins and other symptoms like leg heaviness, aching, or swelling.
Small vein disease is a broader term that refers to dysfunction in these tiny veins, even if the damage isn’t yet visible. In some cases, people may experience symptoms of poor circulation before spider veins appear.
So while spider veins are one form of small vein disease, not everyone with small vein disease will have visible spider veins. That’s why it’s important to schedule an evaluation with a vein specialist, who can determine whether the issue is purely cosmetic or part of a larger circulatory problem.
The Relationship Between Spider Veins and Small Vein Disease
| Feature | Spider Veins | Small Vein Disease |
|---|---|---|
| Location | Tiny veins on or near the surface of the skin | Small veins just below the skin or within deeper tissue |
| Size | Less than 1 mm | 1–3 mm (can include reticular veins) |
| Symptoms | Usually cosmetic; may cause mild burning or itching | Heaviness, fatigue, swelling, or aching legs |
| Cause | Valve weakness, hormonal changes, or increased venous pressure | Chronic venous insufficiency (CVI) in small veins |
| Connection | May be a visible sign of small vein disease | The deeper process that can cause spider veins to form |
In other words, spider veins can develop when small underlying veins begin to malfunction, allowing blood to pool and pressure to build up in the surface veins. Over time, this pressure causes those thin surface veins to become visible as spider veins.
Is Small Vein Disease Associated with Reticular Veins?
Yes, small vein disease and reticular veins are often associated, but they’re not exactly the same condition. Here’s how they relate:
The Connection Between Small Vein Disease and Reticular Veins
-
Reticular veins can develop because of small vein disease in deeper vessels.
-
Both conditions are linked to chronic venous insufficiency (CVI).
-
Treating the underlying reflux in the small veins can often reduce or eliminate reticular veins and prevent progression to varicose veins.
Reticular veins can be a visible symptom or early stage of small vein disease. Both indicate that the veins are under strain and not circulating blood efficiently — which is why evaluation by a qualified vein doctor is essential to prevent worsening symptoms or complications.
Should You be Worried About Reticular Veins?
Diagnosing Small Vein Disease
Because small vein disease is hidden beneath the skin, it can’t always be detected through a simple visual exam. At USA Vein Clinics, specialists use duplex ultrasound imaging to assess blood flow, locate damaged valves, and determine the severity of your condition. This non-invasive test allows your doctor to create a customized treatment plan that targets the exact veins causing your symptoms.
Treatment Options for Small Vein Disease
The good news is that small vein disease is treatable and manageable. Depending on your diagnosis, your vein specialist may recommend:
-
Compression therapy – Wearing medical-grade compression stockings to improve blood flow and relieve swelling.
-
Lifestyle changes – Elevating your legs, maintaining a healthy weight, and exercising regularly can improve circulation.
-
Minimally invasive vein treatments – For persistent cases, procedures such as Endovenous Laser Therapy (EVLT), Radiofrequency Ablation (RFA), or Ultrasound-Guided Sclerotherapy (UGSC) can safely close off diseased veins and redirect blood to healthier ones.
These outpatient treatments typically take less than an hour and allow you to return to your normal activities quickly.
Why Early Diagnosis Matters
Left untreated, small vein disease can progress and damage surrounding tissue. Chronic swelling, skin changes, and venous ulcers can develop, especially near the ankles. By seeking early evaluation from a qualified vein doctor, you can prevent these complications and restore healthy circulation before more serious issues arise.
When to See a Vein Specialist
If you’re experiencing leg pain, swelling, or heaviness—even without visible veins—it’s time to schedule a consultation. A vein specialist can identify the underlying cause and provide a personalized plan to protect your vascular health.